Determining the best support for CRPC patients:
The nurse perspective
The recently-concluded the 21st International EAUN Meeting (EAUN21) provided the latest and most substantial in urological nursing which included the nurse perspective on castration-resistant prostate cancer (CRPC) management.
As a recap, let us define what is CRPC.
CRPC is castrate serum testosterone < 50 ng/dL or 1.7 nmol/L, combined with either of the following:
- Biochemical progression
Three consecutive rises in PSA one week apart resulting in two 50% increases over the nadir, and a PSA > 2 ng/mL - Radiological progression
The appearance of new lesions: either two or more new bone lesions on bone scan or a soft tissue lesion using RECIST (Response Evaluation Criteria in Solid Tumors).
If this is the case standard hormone therapy does not work anymore and the cancer is growing. Prostate cancer (PCa) cells grow in response to stimulation of the androgen receptor.
During androgen suppression therapy, cancer cells find ways to grow despite lower circulating androgen levels. The production of androgen receptors (ARs) rises. The sensitivity of AR to low levels of testosterone increases. There is production of androgens inside the tumour itself.
Now we know that CRPC usually develops during treatment for metastatic disease. The tumour and metastases continue to grow because PCa cells no longer respond to hormonal castration treatment.
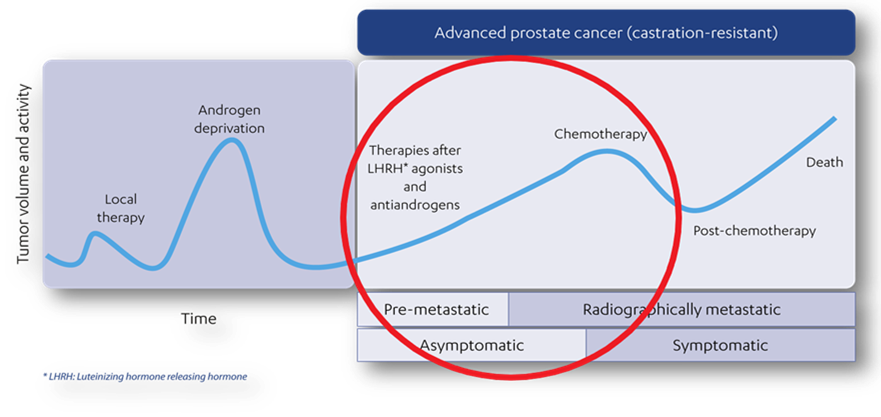
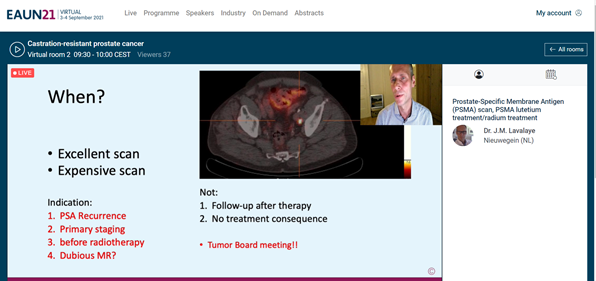
Looking at the timeline seen above, we need to know where we are at with regard to the castration-resistant level i.e. is the patient asymptomatic? To find out, we need to use imaging. For this we need to use the PSMA scan.
After the PSMA scan, a multi-disciplinary team consisting of a nuclear medicine radiologist, a radiologist, an oncologist, a radiotherapist, a pathologist and of course, several urologists will discuss with the patient. Then the best treatment will be determined, depending on whether the patient is asymptomatic or not.
Watchful waiting is an option if the PSA is still low and there are no symptoms nor physical complaints. The aim is to postpone a treatment and therefore side effects from the treatment. The doctor will continue to monitor the patient and if the cancer progresses, one can discuss again what the options are.
The other options as prescribed in my hospital include the following:
- Abiraterone + prednisone, Enzalutamide
- Docetaxel or Radium 223
- PSMA-therapy (is not yet available in the Netherlands, Lutetium-177 therapy)
In addition, treatment with LHRH-(ant) agonist should be continued, as well as, treatment of bone metastasis.
Sometimes patients want time to think whether to start a new treatment or not, and they need assistance in making this decision. In the Netherlands, we have an online CRPC aid that patients can fill out. It has questions such as “What is your aim with this treatment? Is it life extension, reduction of physical complaints, or being able to keep doing what you like doing?”. The patient can discuss the outcome with the oncologist. Then in terms of consultation, the head practitioner moves from the urologist to the oncologist.
What can we do as nurses to support the patients? First of all, the disease itself as well as any treatment can give physical discomfort. If patients call with adverse effects, we make sure that the doctor is informed. The adverse effects we hear the most include fatigue, high blood pressure, bowel movement problems, and retaining fluids. Secondly, we focus on the patient’s well-being e.g. physical, functional, emotional, and social.
In what other aspects do patients need our support as nurses? We do our best to motivate the patients to get fit as much as possible and maintain a healthy lifestyle, if they were not doing so already. We know that being fit can have a positive effect on the quality of life since the treatment can cause many side effects.
We discuss with patients where they need support such as:
- Can they do any type of sports? For example, if they cannot do so due to poor physical condition but are motivated, would they want coaching from a physiotherapist?
- Do they need coaching from a dietician? In the Netherlands, health insurance benefits include a total of 3 hours of collective consultations which can be enough to set patients on the right track.
- Would they benefit from coaching by a psychologist? For some patients, it would be helpful but for some, it may feel like too drastic. If this is the case, we can look into the option of coaching from their general practitioners’ office. In the Netherlands, most general practitioners offices have a psychology nurse amongst the staff.
- For some patients, it is hard to accept that they are in the last stages of PCa. Expressing their feelings and experiences also help the acceptance process. They could benefit from contacting a patient association and fellow patients who are in the same situation.
In addition, do not forget to include the patients’ partners as they are the primary supporter. It is important for them to have a support system and know where to turn to when they feel overwhelmed.
By Nicole Klok, RN, Case Manager, Medical Spectrum Twente (NL)

